
Healthcare Supply Chain Automation: When, Why, and How
Exploring the complex world of healthcare supply chain management and highlighting the importance of automation.
According to recent reports, the global healthcare market is expected to reach $22.57 trillion by 2031, driven by an aging population, advancements in digital health technologies, and a growing emphasis on value-based care. However, despite these advancements, a study found that 72% of healthcare executives acknowledge that siloed and inaccurate patient or member data continues to hinder care quality and disrupt business outcomes, highlighting the urgent need for better data management and system integration.
Healthcare organizations often rely on legacy systems that were not designed to support modern technologies or allow easy integration between critical applications such as Electronic Health Records (EHR), telemedicine platforms, and diagnostic tools. This lack of interoperability poses significant challenges for healthcare providers, hindering operational efficiency, compromising patient care, and slowing the adoption of new technologies.
This article explores a hypothetical case where a healthcare provider successfully navigates complex integration challenges through a comprehensive application modernization strategy, ultimately achieving improved patient care and seamless technology adoption.
Imagine a healthcare provider that has grown significantly in recent years, with an expanding patient base and increasingly complex operations. However, this growth has come with a set of pressing challenges. The provider’s existing applications are disparate, each developed at different times and for different purposes, leading to a fragmented system architecture. These applications are not built for seamless interoperability, making it difficult for different departments and units to exchange data smoothly.
The client also faces significant challenges when attempting to adopt new healthcare technologies, such as electronic health records (EHR) upgrades, telemedicine platforms, and AI-driven diagnostic tools. Their legacy systems are not flexible enough to accommodate these innovations, and the lack of integration slows the implementation of any new technology. Faced with these obstacles, the healthcare provider sought a solution to bridge the gap between its aging infrastructure and the demands of modern healthcare delivery.
Let’s assume that to address these challenges, the healthcare provider turns to a technology modernization partner like rinf.tech capable of delivering a comprehensive solution that ensures seamless system integration while enabling the adoption of cutting-edge technologies. Our modernization approach could be broken down into the following key stages.
The first step in solving integration challenges is a detailed evaluation of the current state of the healthcare provider’s application ecosystem. A strategic technology assessment plays a pivotal role in identifying the areas where integration issues arise and the underlying causes of poor interoperability.
Our team of experts would analyze how the various applications communicate—or fail to communicate—with one another. They would also assess how legacy systems limit providers’ ability to introduce new technologies. This assessment is essential for creating a roadmap that aligns modernization efforts with the healthcare provider’s goals of improving efficiency, reducing operational bottlenecks, and enhancing patient care.
Following the assessment, our engineers will focus on re-architecting the application to address the core issues of system fragmentation and lack of interoperability. The goal is to redesign the application architecture to be more integration-friendly. We would leverage modern architectural frameworks such as microservices and service-oriented architecture (SOA) to ensure that each component of the healthcare system can interact seamlessly with the others.
Microservices allow for greater flexibility, enabling the healthcare provider to scale individual services independently without affecting the entire system. This approach facilitates more accessible updates and better communication between various applications, improving overall system agility. With a service-oriented architecture, the healthcare provider would have a more modular system where different services (such as patient records, billing, and diagnostics) can communicate effortlessly, supporting better data exchange and collaboration across departments.
Application containerization will be implemented to enhance the integration process further. Containerization simplifies the movement of applications across different healthcare environments by encapsulating applications and their dependencies into lightweight, portable containers.
This approach allows the healthcare provider to run applications consistently across different platforms, whether on-premises or in the cloud, ensuring seamless integration of new technologies. By containerizing applications, our team would enable the healthcare provider to adopt modern healthcare tools such as AI-based diagnostics, telehealth solutions, and mobile applications without major disruptions to the existing system. Containers ensure that new tools can be integrated quickly and securely, reducing the time and complexity associated with deployment.
Modernizing healthcare applications is not just about improving integration but is also a key part of a broader digital transformation strategy. Our team solution would align the healthcare provider’s modernized applications with larger digital transformation goals, ensuring that the improvements in interoperability contribute to the overall efficiency and effectiveness of healthcare delivery.
Modernizing the application infrastructure allows the healthcare provider to streamline workflows, automate routine tasks, and introduce advanced analytics for better decision-making. The digital transformation would enhance patient care, reduce administrative overhead, and provide more personalized treatment plans based on real-time data.
With our comprehensive modernization strategy, the healthcare provider would achieve seamless integration across its various systems. The disparate applications would now communicate effectively, creating a unified system where data flows freely between departments, improving coordination and patient outcomes.
The integration-friendly architecture also makes adopting new technologies significantly easier for the healthcare provider. Whether upgrading its EHR system or implementing telemedicine platforms, the provider would no longer face the barriers imposed by legacy systems. This would allow them to stay at the forefront of healthcare innovation, delivering more advanced, personalized patient care.
Additionally, containerization would provide the flexibility to scale and deploy new applications as needed, reducing the time required to bring new services online. This agility is particularly important in the rapidly evolving healthcare landscape, where providers need to adapt quickly to new tools and technologies.
Overall, our solution would lead to improved patient care, more efficient healthcare processes, and a stronger ability to innovate and evolve in an increasingly complex industry.
Modernizing healthcare technology is no longer an option but a necessity for providers aiming to improve patient care, operational efficiency, and system interoperability. As the healthcare landscape continues to evolve—with the increasing need for integrated electronic health records, telemedicine platforms, and AI-driven diagnostic tools—outdated, fragmented systems are no longer viable. Healthcare organizations must prioritize upgrading their infrastructure to keep pace with industry advancements and ensure they can deliver high-quality, patient-centered care.
However, technology modernization in healthcare goes far beyond just improving system integration. A modernized infrastructure allows healthcare providers to harness advanced tools like containerization and cloud-based solutions to improve scalability, enhance data security, and streamline daily operations. By re-architecting applications focusing on microservices and service-oriented architecture, healthcare providers can eliminate the inefficiencies that come with legacy systems and adopt new technologies with greater ease, improving the speed and quality of care.
In the long term, this transformation equips healthcare providers with the tools to future-proof their operations. Moving to a cloud environment, for example, reduces the cost and complexity of maintaining aging systems and provides the flexibility to scale and adapt as patient needs and technological innovations evolve. Continuous integration practices ensure that systems remain updated with the latest advancements, security patches, and features, driving operational resilience and improved patient outcomes.
By embracing technology modernization, healthcare organizations can overcome the integration challenges that hold them back, ensuring seamless communication across systems, enhancing patient care, and positioning themselves as leaders in a rapidly changing healthcare market.
If your healthcare organization struggles with outdated systems and complex integration needs, now is the time to explore how modernization services can transform your infrastructure. Taking proactive steps today can pave the way for a more efficient, secure, and patient-focused healthcare experience
Let’s talk.

Exploring the complex world of healthcare supply chain management and highlighting the importance of automation.

This article explores how healthcare organisations can become more resilient and future-ready by automating and optimizing their supply chain management.
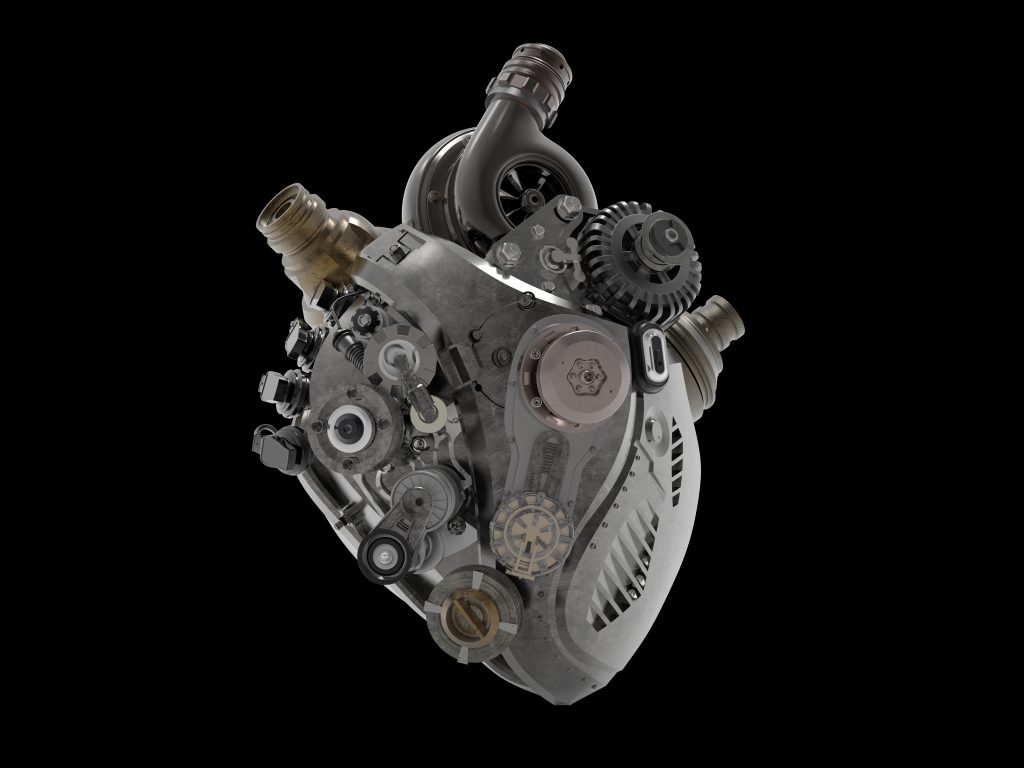
The car of the future is still a conveyance, but more and more an AI supercomputer on wheels, analyzing terabytes of sensor data and making sense of it.